A 34yr OLD MALE PATIENT WITH SOB, SEVERE COUGH AND ANAEMIA
It is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
A 34yr old male patient came with c/o shortness of breath (grade 2) and low grade cough since 20 days
patient is conscious,coherent,cooperative
C/o of severe cough,vomitings and diarrhoea
HISTORY OF PRESENT ILLNESS :
patient was asymptomatic 20 days back then developed breathlessness. SOB (grade2) increased on exertion, relieved on taking rest, decreased on sitting position increased on lying down
After a week he developed intermittent fever during evening time along with vomitings and diarrhoea
Low grade cough
Loss of appetite
Loss of weight
PAST HISTORY
not K/C/O -DM, HTN, EPILEPSY, IHD
H/O bilateral leg ulcers 10 yrs back
PERSONAL HISTORY
Diet :Mixed
sleep:adequate
bowel and bladder movements:regular
Alcoholic regularly
Habits : and chews tobacco
GENERAL EXAMINATION:
patient is concious,coherent,cooperative
Pallor :+ve
Icterus: -ve
Cyanosis: -ve
Vitals:
Tempearture :Afebrile
PP:20CPM
PR: 98BPM
BP:110/80mmhg
SYSTEMIC EXAMINATION
CVS: S1S2 parsystolic murmurs
RS: breating sounds absent
P/A: soft non tender, BS +
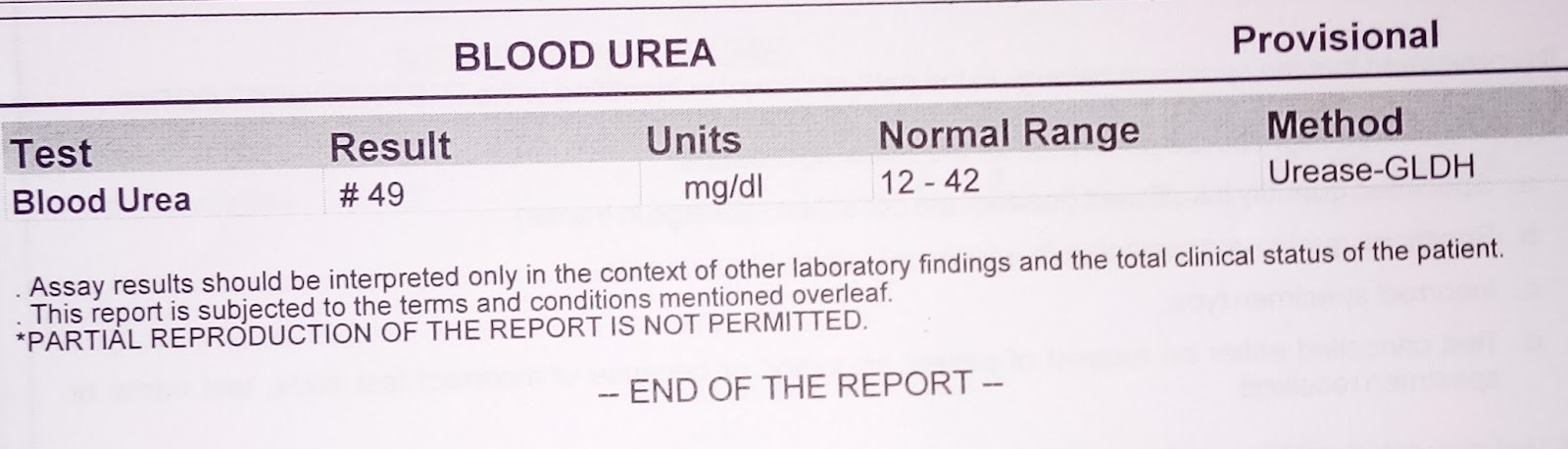
INVESTIGATIONS
RBS: 98mg/dl
HbA1c: 6.5%
COVID-19 : -VE
ESR - 110
C
COLOUR DOPPLER 2D ECHO
DIAGNOSIS :
RIGHT SIDED EMPYEMA
Secondary to TB, CAP
ANEMIA
TREATMENT
INJ. PIPERCILLIN : 2.25g
Inj. Pantaprazole 40mg
Dextromethorphan syrup
Inj Metrogyl500mg TID
ascoril SYP. TID